IS-Instruments has secured funding to develop new instrumentation that leverages advances in Raman spectroscopy to accelerate bowel cancer diagnosis.
Background
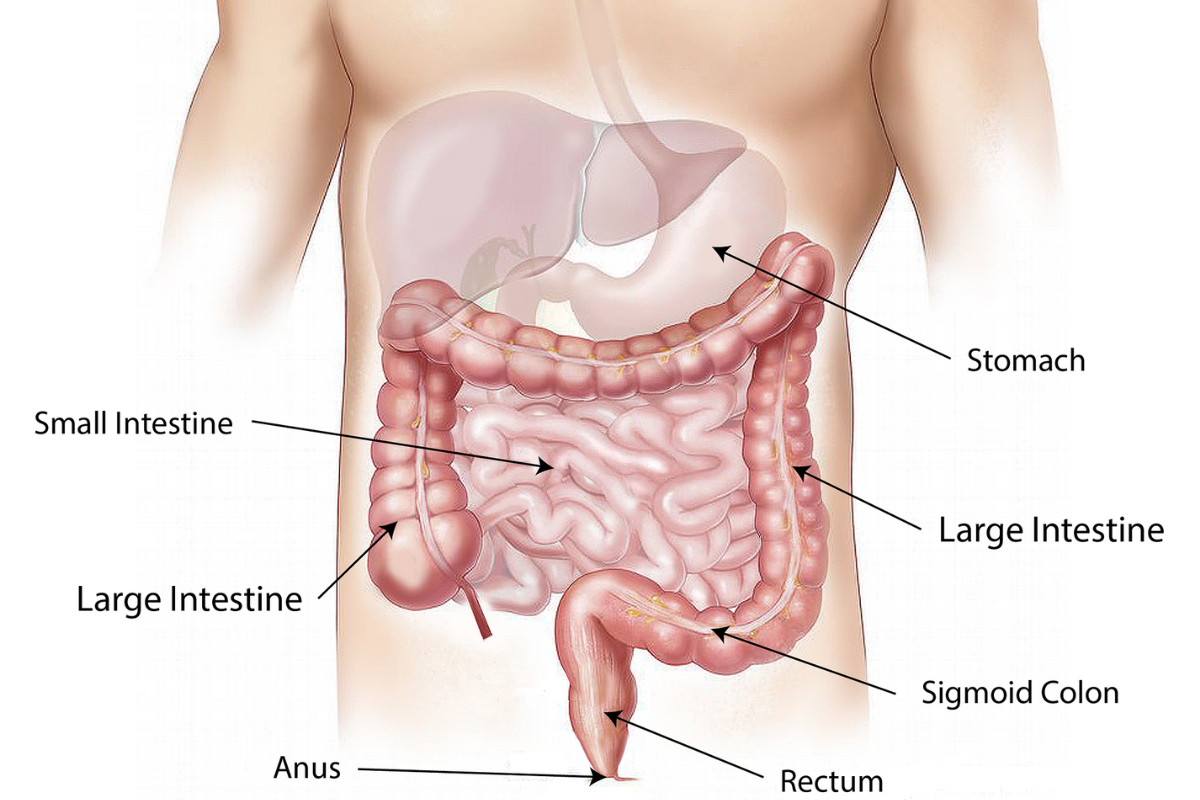
Bowel cancer occurs in the colon or rectum (large intestine), and it is the fourth most common cancer in the UK, with around 40,000 new cases diagnosed each year. About 94% of cases occur in people over 50; however, doctors diagnose more than 2,600 new cases each year in younger individuals.
In the UK, around 268,000 people are living with bowel cancer. Caught early, it is highly treatable through surgery, and the recovery rate is around 50%. However, recurrence is common. (Bowel Cancer UK). Bowel cancer is responsible for 16,600 deaths each year.
Since the 1980s, the UK has seen an increased survival rate for those diagnosed with bowel cancer. This has occurred due to earlier diagnosis and advances in screening, detection, and treatment of cancer. However, the UK still ranks poorly compared with countries with similar socio-economic status and healthcare provision. This is mainly because the UK cannot reliably detect bowel cancer during its earliest and most treatable stages. In 2018 in England, clinicians diagnosed less than 40% of cases at stage 1 or 2 and more than 25% at stage 4. (Bowel Cancer UK, November 2021).
What impact does early diagnosis have on patient survivability? At stage 1, 98% of bowel cancer patients survive for one year or more. At stage 4, only 44% survived for one year or more post-diagnosis. The 5-year net survival rate for patients diagnosed at stage 1 is over 90%, compared to just 10% for those diagnosed at stage 4. Early detection is a key component in treatment and survival rates.
The Long-Term Plan
Published in January 2019, the government laid out the Long-Term Plan for the NHS, which commits to the goals that:
- By 2028, 55,000 more people each year will survive their cancer for five years or more, and
- By 2028, 75% of people with cancer will be diagnosed at an early stage (stage one or two).
Detection is not the only challenge facing the UK: The majority of bowel cancer cases occur in patients over the age of 50, and the UK has a rapidly ageing population. This is placing increasing pressure on already overloaded NHS departments. There is a wide discrepancy in waiting times across the country for gastroenterology units, ranging from 1 to 27 weeks. In 2018, 4,000 patients were waiting longer than the 6-week target for colonoscopy. Additionally, 30% of NHS Trusts were in breach of that target. Therefore, testing methods that reduce waiting times are a crucial element in early diagnosis and successful treatment.
The current method for diagnosis often involves analysing a stool sample for blood, followed by a colonoscopy if the sample indicates it’s necessary. However, doctors cannot yet rely entirely on current stool sample results, so they often perform a colonoscopy for confirmation. Although colonoscopies are also subject to false readings, it is still possible to miss lesions responsible for cancer development. Several novel devices have been introduced to detect flat or depressed tumours or lesions hidden behind folds in the colon. Although advancing technologies continue to enhance diagnostic accuracy, achieving higher reliability requires the development of more sophisticated instrumentation.
Screening and diagnosis methods carry several drawbacks:
- Stool sampling does not always detect blood, an indicator of cancer.
- Current technologies do not reliably and accurately distinguish between cancerous tissue, precancerous adenomas and hyperplastic benign polyps.
- A colonoscopy is a highly invasive and uncomfortable procedure for the patient, requiring sedation.
- During the colonoscopy, a biopsy of suspect tissue is taken and sent for histopathologic analysis.
- Testing can be a lengthy process requiring the involvement of multiple agencies.
- The process is expensive and can be lengthy, and the time taken invariably delays starting treatment.
A Faster Solution
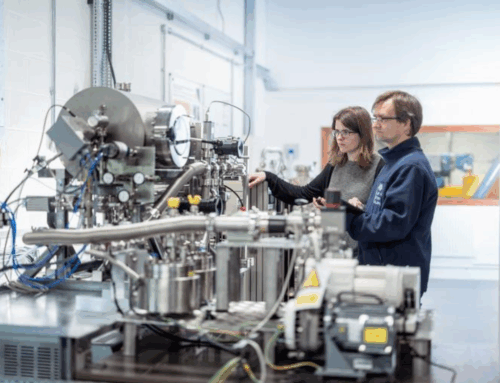
ISI is now involved in a UKRI-funded collaborative project, supported by Innovate UK. The project uses deep UV Raman spectroscopy and machine learning to screen for bowel cancer by analysing tissue and faecal samples (BODICA II).
Project partner, the University of Leeds, has demonstrated that it is possible to correctly identify colorectal cancer from adenomas and normal colonic tissue using Raman spectroscopy. Analysing the tissue samples using machine learning algorithms showed it was possible to distinguish between these tissue types.
Through previous projects, IS-Instruments has developed a deep-UV Raman spectrometer (Odin™) that has demonstrated the ability to detect arthritis in equine synovial fluid. We are currently leading several projects that focus on detecting biomarkers for human diseases and conditions. Through this project, the team aims to develop a clinician-friendly instrument that can identify cancer biomarkers in stool samples. This technology will enable clinicians to determine at the point of testing whether a patient requires further investigation.
Moving forward, the aim is to use the instrument to identify cancerous tissue, precancerous adenomas, and hyperplastic benign polyps within the endoscopy suite in a few minutes, rather than sending samples away for testing, which would incur further expense and delays. If successful, the instrument would represent a viable alternative to current diagnostic methods, significantly speeding up and simplifying the process. It has the potential to save more lives through earlier diagnosis and treatment, and will result in substantial cost savings.
BODICA II is due to run until October 2025.
UKRI project reference 10067160.