IS-Instruments has won funding to develop new instrumentation exploiting advances in Raman spectroscopy to speed up bowel cancer diagnosis.
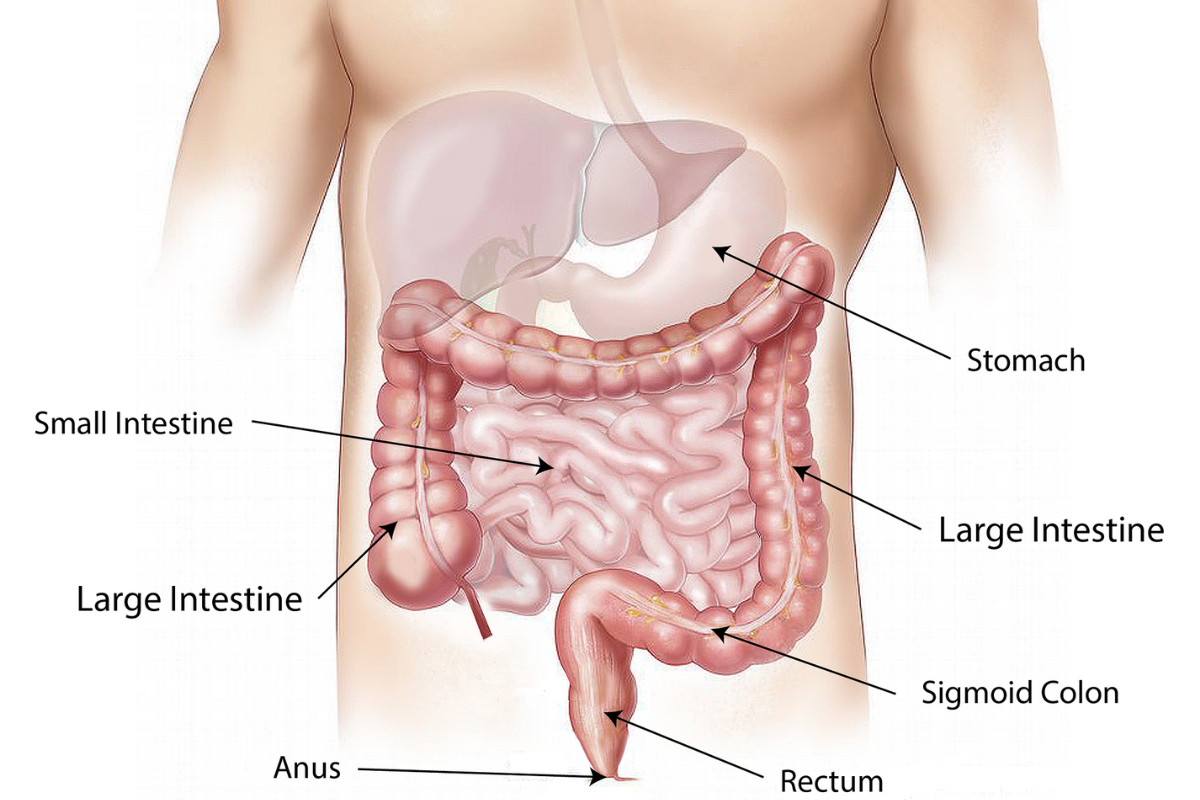
Bowel cancer occurs in the colon or rectum (large intestine), and it is the fourth most common cancer in the UK, with around 40,000 new cases diagnosed each year. Around 94% of those are in people over the age of 50; however, more than 2,600 new cases are diagnosed yearly in people under that age. In the UK, around 268,000 people are living with bowel cancer. Caught early, it is highly treatable through surgery, and the recovery rate is around 50%. However, recurrence is common. (Bowel Cancer UK). Bowel cancer is responsible for 16,600 deaths each year
Since the 1980s, the UK has seen an increased survival rate for those diagnosed with bowel cancer. This has come about due to earlier diagnosis and innovation in methods for screening for, detecting, and treating cancer. However, the UK still ranks poorly compared with countries with similar socio-economic status and healthcare provision. This is mainly because the UK still lacks the ability to reliably detect bowel cancer during its earliest and most treatable stages. In 2018, in England, less than 40% of cases were diagnosed at stage 1 or 2, and over 25% were diagnosed at stage 4 (Bowel Cancer UK, November 2021).
What impact does early diagnosis have on patient survivability? At stage 1, 98% of bowel cancer patients survive for one year or more. At stage 4, only 44% survived for one year or more post-diagnosis. The 5-year net survival for patients diagnosed at stage 1 is over 90%, compared to just 10% at stage 4. Clearly, early detection is a key component in treatment and survival rates.
Published in January 2019, the government laid out the Long-Term Plan for the NHS, which commits to the goals that:
- by 2028, 55,000 more people each year will survive their cancer for five years or more and
- by 2028, 75% of people with cancer will be diagnosed at an early stage (stage one or two).
Detection is not the only challenge facing the UK: The majority of bowel cancer cases occur in patients over the age of 50, and the UK has a rapidly ageing population. This is placing increasing pressure on already overloaded NHS departments. There is a wide discrepancy in waiting times around the country for gastroenterology units, ranging from one to twenty-seven weeks. In 2018, 4,000 patients were waiting longer than the 6-week target for colonoscopy, with 30% of NHS Trusts in breach of the same target. Therefore, testing methods that reduce waiting times are a crucial element in early diagnosis and successful treatment.
The current method for diagnosis often involves an analysis of a stool sample for the presence of blood, followed by a colonoscopy if the stool sample indicates it’s necessary. However, current stool sample results are not 100% reliable, and a colonoscopy is often required, although colonoscopies are also subject to false readings: it is still possible to miss lesions responsible for cancer development. Several novel devices have been introduced to find flat or depressed tumours or lesions hidden behind folds in the colon. Although some technologies are improving diagnosis rates, more sophisticated devices are required.
Screening and diagnosis methods carry a number of drawbacks:
- Stool sampling does not always detect the presence of blood, an indicator of cancer.
- Current technologies do not reliably and accurately distinguish between cancerous tissue, precancerous adenomas and hyperplastic benign polyps.
- A colonoscopy is a highly invasive and uncomfortable procedure for the patient, requiring sedation.
- During the colonoscopy, a biopsy of suspect tissue is taken and sent for histopathologic analysis.
- Testing can be a lengthy process requiring the involvement of multiple agencies.
- The process is expensive and can be lengthy, and the time taken invariably delays starting treatment.
A faster solution is being sought.
ISI is now involved in a collaborative UKRI project funded by Innovate UK. The project uses deep UV Raman spectroscopy and machine learning to screen for bowel cancer using tissue and faecal sample analysis (BODICA II).
Project partner, the University of Leeds, has demonstrated it is possible to correctly identify colorectal cancer from adenomas and normal colonic tissues using Raman spectroscopic techniques. Analysing the tissue samples using machine learning algorithms showed it was possible to distinguish between these tissue types.
Through previous projects, IS-Instruments has developed a deep UV Raman spectrometer (Odin), which has demonstrated the ability to detect arthritis in equine synovial fluid and is currently involved in other projects to detect markers for human diseases and conditions. This project aims to develop a clinician-friendly instrument that can detect cancer biomarkers in stool samples, informing the clinician at the point of testing whether further investigation is warranted. Moving forward, the aim is that the instrument could then be used to identify cancerous tissue, precancerous adenomas and hyperplastic benign polyps within the endoscopy suite in a few minutes rather than having to send samples away for testing, incurring further expense and delays. If successful, the instrument would represent a viable alternative to current diagnostic methods, speeding up and simplifying the process significantly, saving more lives through earlier diagnosis and treatment, and resulting in substantial cost savings.
BODICA II is due to run until October 2025.
UKRI project reference 10067160.